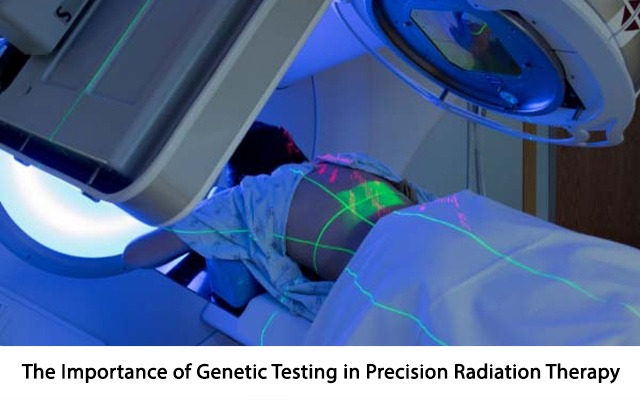
Radiation oncology has long been a part of cancer treatment, helping millions of patients battle a variety of tumours. However, the approach to radiation therapy has evolved significantly in recent years, thanks to advancements in genetics and molecular biology.
One of the most promising developments in this field is the integration of genetic testing into precision radiation oncology. This approach tailors radiation treatments to individual genetic profiles, improving outcomes while minimising side effects. But why is genetic testing so crucial in modern radiation oncology? Read on to know more.
Role of Genetic Testing in Precision Radiation Oncology
1. Personalized Treatment Plans
Traditional radiation therapy often uses standard dosages and treatment plans based on the type and location of the cancer. While effective for many patients, this approach does not account for the unique genetic characteristics of each tumour or patient. Cancer is a highly heterogeneous disease, meaning the same cancer type can behave very differently from person to person. By incorporating genetic testing into radiation oncology, doctors can identify specific mutations or genetic markers that might influence how a patient’s tumour responds to radiation.
Genetic testing allows oncologists to create more personalised treatment plans. For example, genetic testing can uncover alterations in DNA repair mechanisms, such as mutations in the BRCA1 or BRCA2 genes, which could make certain cancers more sensitive to radiation. Conversely, if a tumour has genetic mutations that make it more resistant to radiation, doctors can adjust the radiation dose or even combine it with other treatments, such as targeted therapies, to improve its effectiveness.
2. Identifying Tumour Radiosensitivity
One of the most significant advantages of genetic testing in precision radiation oncology is its ability to predict tumour radiosensitivity. Some tumours are more sensitive to radiation because of genetic mutations that impair their ability to repair radiation-induced DNA damage. Conversely, other tumours may possess mutations that make them more resistant to radiation, meaning they require higher doses or a different kind of radiation therapy.
Through genetic testing, doctors can better assess a tumour’s inherent sensitivity to radiation. This information is critical for avoiding over-treatment in cases where tumours may not need high radiation doses, reducing unnecessary side effects. In contrast, resistant tumours can be treated more aggressively, ensuring that the radiation is optimised for the best possible outcome.
3. Improving Quality of Life
Radiation therapy can be accompanied by significant side effects, like fatigue, skin irritation, and damage to healthy tissues. However, genetic testing can help identify patients who may be at greater risk for radiation-induced side effects based on their genetic makeup. For example, some genetic variations can affect how the body metabolises radiation or repairs radiation-induced damage. By identifying these variations beforehand, doctors can adjust radiation doses or modify the treatment plan to minimise harm to healthy tissues. This improves the patient’s quality of life during and after treatment.
Additionally, genetic testing can detect genetic predispositions to long-term radiation toxicity, like fibrosis or cardiovascular complications, allowing doctors to adopt more cautious, well-informed treatment strategies.
The Future of Precision Radiation Oncology
As our understanding of genetics and cancer biology continues to grow, the role of genetic testing in radiation oncology is likely to expand. Advances in next-generation sequencing and molecular profiling technologies are making genetic testing more accessible and affordable, which will enable clinicians to incorporate genetic information into treatment decisions for more patients. By combining genetic data with advanced imaging techniques as well as artificial intelligence, oncologists can design even more precise, personalised radiation therapies that deliver maximum benefit with minimal harm.
Conclusion
Genetic testing is becoming an indispensable tool in precision radiation oncology. It enhances the personalization of treatment plans and helps predict tumour response to radiation. This ultimately improves patient outcomes. As the field continues to evolve, the integration of genetic testing into routine clinical practice holds the promise of transforming cancer care, offering hope for better, more targeted treatments. Reach out to the best precision oncologist in Kolkata if you want to know more about genetic testing in precision radiation oncology.